



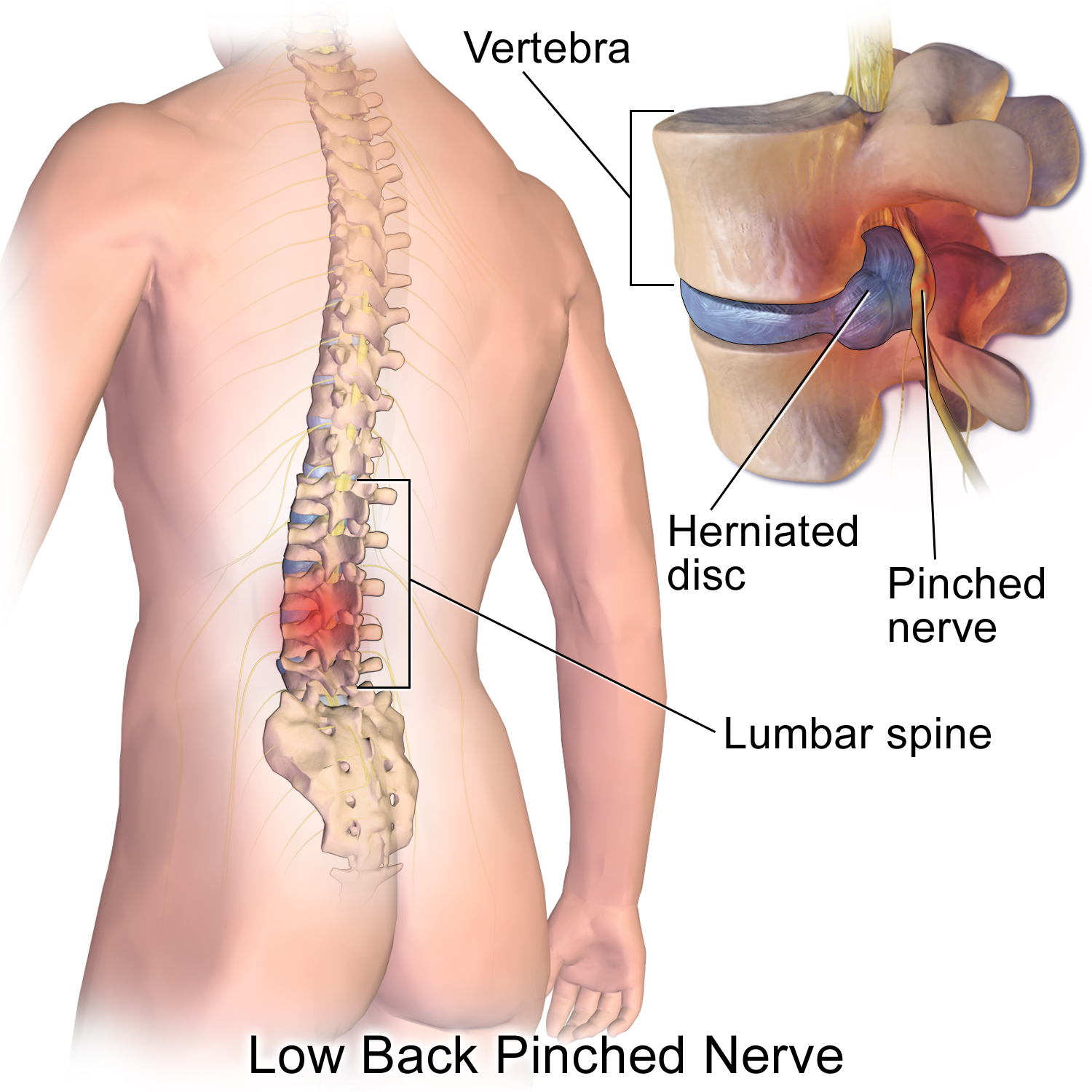
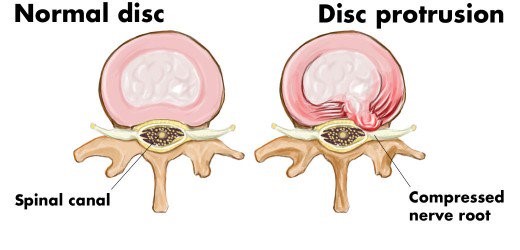
Spinal disc herniation or a slipped disc, is a condition in which there is a tear in the outer fibrous ring of an intervertebral disc allowing the soft, central portion to bulge out and cause compression on nerves/spinal cord. This tear in the disc ring may result in the release of chemicals causing inflammation, which may directly cause severe pain even in the absence of nerve root compression. The majority of spinal disc herniation cases occur in the lumbar region. The second most common site is the cervical region. The thoracic region disc prolapses are extremely rare.
Disc herniation usually occurs due to age-related degeneration, trauma, after lifting heavy objects or straining. Disc herniations can be a worsening of a previously existing disc protrusion, a condition in which the outermost layers of the anulus fibrosus are still intact, but can bulge when the disc is under pressure.
Disc herniations can result from general wear and tear, such as constant sitting or squatting, driving, or a sedentary lifestyle. Professional athletes, especially those playing contact sports are prone to disc herniation.
Herniations usually occur posterolaterally, where the anulus fibrosus is relatively thin and is not reinforced by ligaments.
Symptoms of a herniated disc can vary depending on the location of the herniation. They can range from little or no pain if the disc is the only tissue injured, to severe and unrelenting neck pain or low back pain that will radiate into the regions served by affected nerve roots that are irritated by the herniated material. Pain from a herniated disc is usually continuous or at least is continuous in a specific position of the body.
Other symptoms may include
It is possible to have a herniated disc without any pain or noticeable symptoms. If the extruded nucleus pulposus material doesn't press on soft tissues or nerves, it may not cause any symptoms.
Lumbar disc herniation occurs in the lower back, usually between L4-5, L5-S1 level. A prolapsed disc in the lumbar spine can cause radiating nerve pain. This type of pain is usually felt in the lower extremities or groin area. Radiating nerve pain caused by a prolapsed disc can also cause bowel and bladder disturbances.
Symptoms can affect the lower back, buttocks, thigh, anal/genital region, and may radiate into the foot and/or toe. The sciatic nerve is the most commonly affected nerve, causing symptoms of sciatica. Patient may also experience a numb, tingling feeling throughout one or both legs and even feet or even a burning feeling in the hips and legs.
Typically, symptoms are experienced only on one side of the body. If the prolapse is very large and presses on the nerves within the spinal column or the cauda equina, both sides of the body may be affected.
Compression of the cauda equina can cause permanent nerve damage or paralysis. The nerve damage can result in loss of bowel and bladder control as well as sexual dysfunction. This disorder is called cauda equina syndrome.
Other complications include chronic pain.
Cervical disc herniations occur in the neck, most commonly at C5-6/C6-7 levels. It may be associated severely debilitation compressive myelopathy.
Symptoms include pain at back of the skull, the neck, shoulder, scapula, arm & hand. The nerves of the cervical plexus and brachial plexus can be affected.
Diagnosis of disc prolapse is made by based on the history, symptoms and physical examination. Sometimes special tests may be performed to confirm or rule out other causes of symptoms such as spondylolisthesis, degeneration, tumours, metastases and space-occupying lesions, as well as to evaluate the efficacy of potential treatment options.
Physical examination
The straight leg raise may be positive, as this finding has low specificity.
Imaging
Projectional radiography (X-ray imaging): They are used to exclude other possibilities such as tumors, infections, fractures, etc.
Computed tomography scan (CT or CAT scan): It can show the shape and size of the spinal canal, its contents, and the structures around it, including soft tissues. However, visual confirmation of a disc herniation can be difficult with a CT.
Magnetic resonance imaging (MRI): It can show the spinal cord, nerve roots, and surrounding areas, as well as enlargement, degeneration, and tumors. It shows soft tissues better than CT scans. An MRI provides the most conclusive evidence for diagnosis of a disc herniation.
Electromyogram and nerve conduction studies (EMG/NCS): Measures electrical impulse along nerve roots, peripheral nerves, and muscle tissue, which can be used to indicate any abnormalities and to pinpoint sources of nerve dysfunction distal to the spine.
Human Brain is an extremely complex organ that controls all the functions of our body. Immediate medical attention is read more
Tumours are abnormal tissues which cells grow & multiply uncontrollably, causing dysfunction of the organ from which it read more
Stroke refers to a condition in which there is reduced blood flow to the brain resulting in injury to brain cells causing permanent read more
The spinal cord is connection between the brain and peripheral nervous system and is protected by bones - spinal vertebra. read more
Spinal disc herniation or a slipped disc, is a condition in which there is a tear in the outer fibrous ring of an intervertebral read more
The Peripheral Nervous System consists of the nerves outside the brain and spinal cord. Disorders of the peripheral nervous read more