

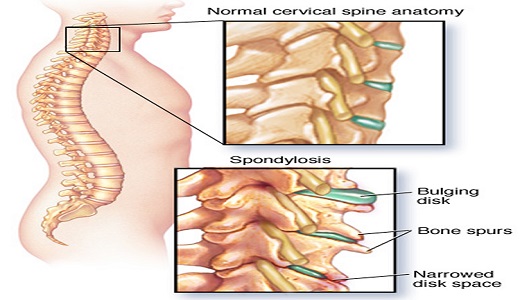
Spondylosis is a type of arthritis spurred by wear and tear to the spine. It happens when discs and joints degenerate, when bone spurs grow on the vertebrae, or both. These changes can impair the spine's movement and affect the nerves and other functions.
Cervical spondylosis is the most common type of progressive disorder that affects the neck during aging.
Other types of spondylosis develop in different parts of the spine:
The effects of spondylosis vary among individuals, but they do not usually cause serious problems.
When a person has symptoms, these are often pain and stiffness that tend to come and go.
Spinal osteoarthritis is another term for spondylosis. Osteoarthritis describes arthritis that results from wear and tear. It can affect any joint in the body.
Symptoms can include weakness and tingling in the limbs.
Most people with age-related spondylosis do not experience any symptoms. Some people have symptoms for a while, but then they go away. Sometimes, a sudden movement can trigger symptoms.
Common symptoms are stiffness and mild pain that gets worse following certain movements or long periods without moving, while sitting for a long time, for example.
More severe symptoms include:
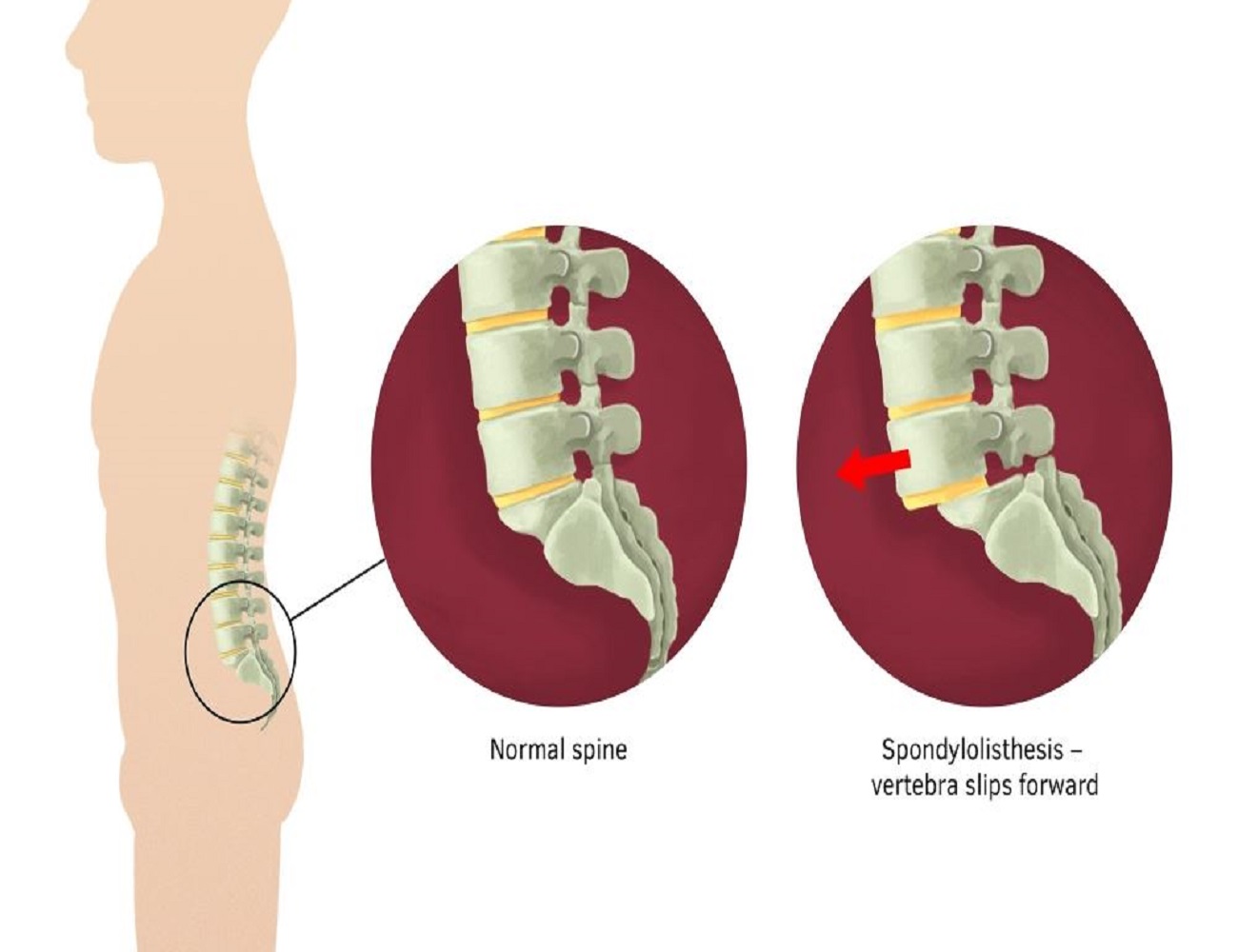
Spondylolisthesis occurs when one of the vertebrae in the spine slips out of position.
Usually, this vertebra has slid forward over the vertebra directly below it. Spondylolisthesis is most common in the lower back, and occurs more often in adolescents and adults.
Due to the varying degrees and causes of the misalignment, spondylolisthesis is broken down into types and grades. The six main types are based on the cause of the spondylolisthesis.
Type I - In some cases, people are born with spondylolisthesis. A child may also develop the condition naturally during his or her developmental years. In both cases of Type I spondylolisthesis, a child may not experience any symptoms or problems until later in life.
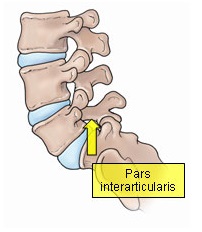
Types II - In Type II, the most common type, there is a problem with a section of the vertebra called the pars interarticularis. Type II is further broken down into the following subtypes:
The fractures from Type II only become spondylolisthesis if they cause the vertebra to slip forward.
Type III - Type III is associated with aging and the natural wear and tear on a person's body.
Type IV - Type IV is a fracture that occurs anywhere in a vertebra except in the pars interarticularis region.
Type V - Type V involves tumors on the vertebrae that push on the bones and cause weakness.
Type VI - Type VI is an uncommon spondylolisthesis caused by weakening of the back due to surgery.
Spondylolisthesis is further classified into grades, according to how far out of place the vertebra is. The grades are:
A person may have had spondylolisthesis since birth and never experienced any symptoms from it. It is common for a person to develop symptoms as they age, however.
Symptoms can range in severity from non-existent to a loss of urination and bowel movement control in more severe cases.
Some of the most common symptoms include:
Adolescent back pain has been reported to affect more than 50% of school age patients. Parents are often confounded by the severity of the complaints and yet their teenager continues in sports or other extracurricular activities. After months of complaints and minimal relief of symptoms with anti-inflammatory drugs, the family will seek an evaluation.
The adolescent with lumbar back pain may have multiple reasons other than overuse or "growing pains" for the discomfort.
The clinical examination provides information about the location of the pain, muscle spasm, lumbar spine range of motion, hamstring muscle tightness, muscle strength in the legs, reflexes, and sensation in the legs.
X-ray studies may discount several of the potential diagnoses and direct the physician to propose the diagnosis of a pars interarticularis stress injury or fracture.
The pars interarticularis is a portion of the lumbar spine that joins the upper and lower joints together. The pars is normal in the vast majority of children. Certain patients begin to experience abnormal growth and development of this particular region in the bone. A genetic weakness to the bone has only been established in certain ethnic groups such as Alaskan Indians. It does appear that certain athletic activities or injuries (gymnastics, heavy weight lifting) may result in problems in susceptible individuals.
There are three stages of injury to the pars interarticularis:
Stress reaction or injury may occur when the bone experiences excessive wear and tear from activities of daily living, sports or a fall. The symptoms may include lumbar pain, stiffness and hamstring muscle tightness. X-rays will not reveal any abnormality. A bone scan will demonstrate the inflammation in the pars. Treatment consists of relieving the pain and restoring spinal flexibility. After several months, the majority of patients resume most activities.
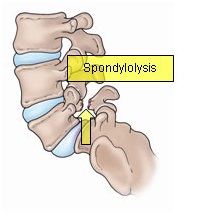
If the pars "cracks" or fractures, the condition is called Spondylolysis. The x-ray confirms the bony abnormality. Treatment is customized based on the severity of symptoms. Anti-inflammatory drugs, physical therapy, brace wear, and activity modifications will be considered. core exercisesPrior to a release to activities after the pain resolves, a course of truncal core muscle strengthening (pilates or yoga) may be prescribed to condition the muscles and minimize reinjury.
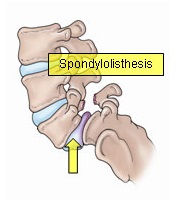
If the fracture gap at the pars widens, then the condition is called Spondylolisthesis. Widening of the gap leads to the fifth lumbar vertebra shifting forward on the part of the pelvic bone called the sacrum. Standing lateral spine x-rays are measured to determine the amount of forward slippage.
Treatment is prescribed to decrease any acute spasm and restore spinal flexibility. One of the mainstays of physical therapy treatment is to perform truncal core strengthening exercises. The therapist will caution the patient on avoiding hyperextension maneuvers and excessive abdominal "crunches".
Prognosis is affected by the amount of slippage. In general, most patients with less than 50% slippage fend to fare well through adolescence. With slippage of 50% or greater, the potential for additional slippage with growth and aging is greater. The small numbers of patients who do not respond to conservative medical management are evaluated for a spinal fusion.
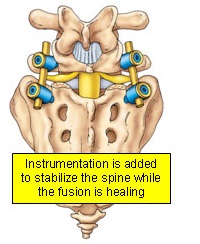
If the pain, spasm, or slippage increases, then the surgeon will discuss several potential surgical options. For a majority of children, fusing the 5th lumbar vertebra to the sacrum is the first choice. The fusion involves removing the loose bony fragments and placing bone graft in such a manner that will lead to the successful "gluing together" of the two vertebra.
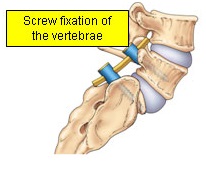
The patient is restricted postoperatively with a cast or brace until healing is complete. In older patients the alignment of the two vertebra may benefit from the addition of bone screws during the healing process.
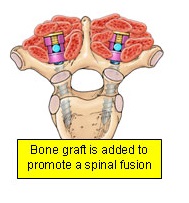
Bone graft is still added to promote a fusion that may take up to three to six months to heal completely. After a successful fusion most athletic activites can be enjoyed once again.
Human Brain is an extremely complex organ that controls all the functions of our body. Immediate medical attention is read more
Tumours are abnormal tissues which cells grow & multiply uncontrollably, causing dysfunction of the organ from which it read more
Stroke refers to a condition in which there is reduced blood flow to the brain resulting in injury to brain cells causing permanent read more
The spinal cord is connection between the brain and peripheral nervous system and is protected by bones - spinal vertebra. read more
Spinal disc herniation or a slipped disc, is a condition in which there is a tear in the outer fibrous ring of an intervertebral read more
The Peripheral Nervous System consists of the nerves outside the brain and spinal cord. Disorders of the peripheral nervous read more